An international team of researchers reported that detecting the activity of the enzyme beta-secretase (β-Site Amyloid Precursor Protein–Cleaving Enzyme 1, BACE1) in the blood could predict the development of Alzheimer’s disease (AD) at an early clinical stage as well as the progression of the disease from the first symptoms of mild cognitive impairment (MCI) to AD dementia. Professor SHEN Yong, University of Science and Technology of China (USTC) and his colleagues performed the study on a total of 224 individuals recruited from three independent international academic AD research centers and memory clinics (recruited in the US, Germany and Sweden). Three age-matched multi-site study cohorts were assembled as follows: 75 probable AD patients, 96 MCI subjects, and 53 age- and sex-matched healthy controls.
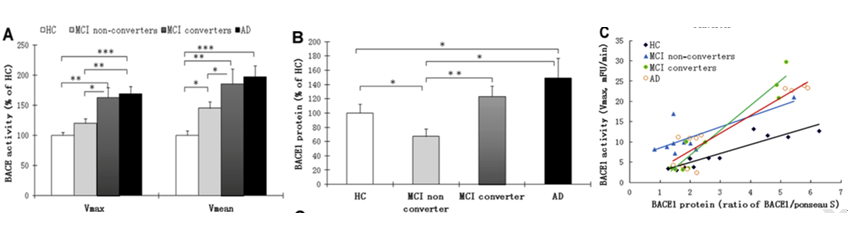
Generally, BACE1 is thought to be central in AD pathophysiology. It is highly expressed during development, as well as in diseased neurons. Processing amyloid precursor protein (APP) through this enzyme contributes to Ab production and amyloid plaque formation in AD brains. Shen, Li and Hampel and collaborators previously reported elevated levels of BACE1 in brains and cerebrospinal fluid (CSF) of patients with AD (Yang et al., Nature Medicine, 2003; Zhong et al., JAMPA Psychiatry, 2007). In the current study, Shen and his colleagues found elevated blood concentrations of BACE1 also during the progression of the disease in AD patients and MCI subjects. [Courtesy of Shen et al., 2017. ©Biological Psychiatry.]
(Image by SHEN Yong)
They showed that blood (plasma) BACE1 activity was significantly increased in MCI subjects, primarily in individuals who progressed to AD, and in subjects with probable AD. The increase of BACE1 activity in A patient was also correlated with a worsening on the AD clinical cognitive rating scale, namely the Mini-Mental State Examination (MMSE) score. “Our results suggest that BACE1 activity may complement the evolving array of AD biomarkers for early detection, diagnosis and dissection of AD and can be a powerful tool to track disease progression”, saida senior author of the study Dr. Harald Hampel, Pierre and Marie-Curie University, Paris, France.Instead of utilizing CSF for the diagnosis of AD, the ability of investigating blood biological alterations related to the development of AD offers a relevant advantage.
This work is published as “Increased Plasma Beta-Secretase 1 May Predict Conversion to Alzheimer's Disease Dementia in Individuals With Mild Cognitive Impairment” in the upcoming 2017 of Biological Psychiatry online (IF=11.212). And it’s coauthored by Professor SHEN Yong, University of Science and Technology of China (USTC), Neurodegenerative Disease Research Centre (NDRC) in Hefei, China, Professor Rena Li, Director of Center for Hormone Advanced Science and Education, Roskamp Institute, Florida, United State, and Professor Harald Hampel of Sorbonne Universities, Pierre and Marie-Curie University (UPMC) and AXA Research Fund and UPMC Chair on Alzheimer's disease, Paris, France and other researchers from these labs.
Yong Shen, Harald Hampel, and colleagues are working with the Clinical Neuroscience Research in AD consortium to reproduce this data in a larger cohort. The consortium’s Phenotype-Genotype-Biomarker study collects blood and CSF samples from AD patients and MCI subjects every six to twelve months while clinically assessing cognitive and behavioral symptoms. In the next step, they will use the Paris monocenter INSIGHT-preAD study to investigate asymptomatic preclinical at risk individuals stratified by amyloid PET.
Link of the paper:
http://www.biologicalpsychiatryjournal.com/article/S0006-3223(17)30098-7/fulltext
Contact
Prof. SHEN Yong
yongshen@ustc.edu.cn
http://biox.ustc.edu.cn/szdw/szcjxz/201501/t20150115_209482.html